Is Your Stamina Off After Being Sick? Your Breathing Muscles Might Be the Reason
As We Move from Cold and Flu Season to Allergy Season …
The Surprising Muscle Group Affected by Respiratory Conditions
Once you recover from an illness you may still be fatigued and not sleeping so well. Most people do not attribute those things to the lasting impact on your muscles from being sick.
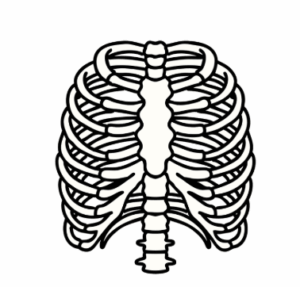
Allergies, bronchitis, pneumonia … they don’t just affect your lungs. They wear down your muscles — specifically, the intercostals muscles in your chest.
These stealth muscles connect your ribs, expanding and contracting up to 30,000 times a day as you breathe. They don’t get a break — and after prolonged allergies or illness, they can tighten and get stuck in “protect mode.”
 Why Breathing Still Feels Hard After You’ve Recovered
Why Breathing Still Feels Hard After You’ve Recovered
Persistent, forceful coughing—common with most respiratory illnesses—can overwork your intercostal muscles. And unlike overuse of your arm or leg muscles, you can’t just stop using the intercostals to let them rest. You still need to breathe.
Over time, the muscles tighten and lose their flexibility. Even after you’re “better,” your breath may still feel shallow or off.
Fatigue, poor sleep, and reduced stamina often follow — and many people never connect it to issues with the mechanics of their breathing. That’s exactly what happened to Karen.
Karen’s Story: Still Exhausted Weeks After Pneumonia
Karen (yes, that’s her real name — and she’s my neighbor!) recently had a virus which resulted in a case of pneumonia. Antibiotics cleared the infection, but she still couldn’t shake the exhaustion.
As an avid tennis player, she was surprised that even walking a block left her wiped out. The idea of getting back on the court seemed impossible.
I invited her for a session to see how Bridging would help. The results were immediate!
During Karen’s session, we used the Bridging® Technique to gently support her chest muscles which allowed the movement in her rib cage to relax. This support gave her intercostal muscles the break they needed to start moving again and exit “protect mode.”
You can see the entire process and resulting changes in the short video in the link below.
Once reset, the action of breathing keeps the intercostal muscles pliable and moving until they are injured or sick again. This is why the changes with Bridging last — the movement from breathing sustains the resets.
A better recovery is that simple, yet that specific.
(Yes, there are some physics principles in play related to pressurization and coordination from the support compression, but I won’t bore you with those nerdy details.)
Something Else Changed for Karen too!
In addition to the relaxed and expanded breathing, a change was also audible. Karen’s voice, initially gravelly and weak, became clearer and stronger as her breathing expanded.
The video team even had to adjust the audio settings because she started speaking so much louder!
Analogy: A Balloon in a Small Box
 A great way to think about the implications of stuck intercostals to breathing is as follows:
A great way to think about the implications of stuck intercostals to breathing is as follows:
Consider a balloon. You blow it up to its full size. You want to take it to a friend for a surprise and find a box to put it in. The box is too small so you let some air out to fit inside the box. The balloon size is limited by the box.
This is what happens when the ribs lose their ability to expand. Your lungs are not able to expand as much as previously, so you’re taking smaller breaths without realizing it.
Get Back to Breathing — and Living — Fully
The Bridging Technique is a gentle, fast-acting way to reset your muscle coordination after illness, surgery, or stress. You’ll breathe easier, sleep better, and feel more like yourself again.
What’s involved:
- Assessment of movement flow in your core and limbs
- Problem-solving to uncover hidden movement restrictions
- Gentle resets that restore how your muscles support breathing and balance
Results are fast. The process is gentle. Changes last.

